
MEDEX is proud to have earned URAC accreditation for Utilization Management. The designation demonstrates MEDEX is dedicated to quality and safety.
Although Utilization Review is known to be one of the most effective cost containment tools within the Workers’ Compensation industry, unfortunately the cost of UR can outweigh the benefit.
Offering a simple solution to this complicated process, MEDEX can provide the most highly managed and cost effective UR services currently available in the industry, with state-of-the-art systems, efficient processing, and consistent results.
MEDEX will automate the application of specific, proven medical protocols, based on ICD10 codes, in a consistent and timely manner. Using an automated review system, MEDEX will decrease the cost and timeframe associated with approving the most common requests received. MEDEX will apply medical resources only where and when necessary, not on every request!
MEDEX will determine if treatment requests are from network providers if appropriate, and will integrate with Claims and Bill Review processes. Learn the facts on the true costs and net savings of an effective program. Experience the benefits of our commitment to excellence and quality service.
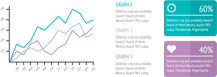
Cost Effective Utilization Management:
MEDEX specializes in administering cost containment programs to help reduce Workers’ Compensation claim costs.
For a more in depth look at the benefits that MEDEX can provide, take a look at our case studies!
California law requires employers to pay for all appropriate medical treatment for on-the-job injuries.
To report provider listing inaccuracies, contact the MPN contact at 1-877-775-7772 or mpnhelp@medexhco.com
To contact the MPN contact, call 1-877-775-7772 or mpnhelp@medexhco.com
To contact the Medical Access Assistant, call 1-888-509-1474 or MAA@medexhco.com
To obtain a copy of any notification regarding the MPN, including the Complete Employee Notification, please contact the claims administrator for your claim. If you need assistance identifying or contacting the claims administrator on your claim, please contact the Medical Access Assistant at 1-888-509-1474 or MAA@medexhco.com. We may be able to help you connect to the appropriate party.
© 2016-2025 MEDEX · MEDEX The Total Solution to Rising Workers' Compensation Costs
Conditions of Use • Privacy Policy

