 Exploring Azithromycin Resistance: Causes and Solutions
Exploring Azithromycin Resistance: Causes and Solutions
Understanding Azithromycin Resistance in Bacteria
Azithromycin resistance in bacteria is a growing concern in the medical field. It is crucial to comprehend the mechanisms behind this phenomenon to effectively combat its implications on public health. The development of resistance is a complex process that involves genetic mutations and selective pressure from antibiotic use. By understanding how bacteria evolve to resist azithromycin, healthcare professionals can devise strategies to mitigate its impact and preserve the effectiveness of this essential antibiotic.
| Factors Contributing to Azithromycin Resistance | | -------------------------------------------------- | | Genetic Mutations in Bacteria | | Overuse and Misuse of Antibiotics | | Inadequate Antibiotic Stewardship Practices |
Factors Contributing to the Development of Resistance

Factors Contributing to the Development of Resistance:
Azithromycin resistance in bacteria can be attributed to a complex interplay of various factors, ranging from overprescription of antibiotics to misuse and overuse in both human and veterinary medicine. One significant driver of resistance is the inappropriate or incomplete course of treatment, which can lead to the survival and proliferation of resistant bacterial strains. Additionally, the widespread use of azithromycin in industrial farming practices, where it is often administered as a growth promoter rather than for therapeutic purposes, has also been linked to the emergence of resistance. Poor infection prevention and control measures in healthcare settings further exacerbate the problem, allowing for the transmission of resistant bacteria among patients and healthcare workers.
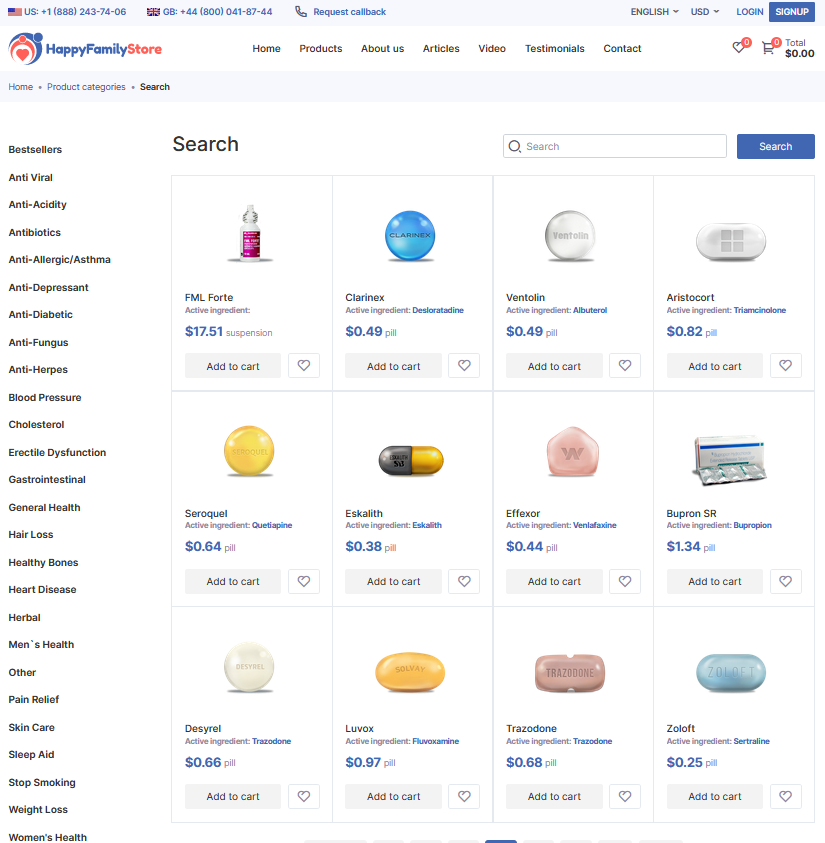
The availability of azithromycin without a prescription in certain regions also contributes to resistance, as improper self-medication practices can lead to suboptimal dosing or treatment durations. Furthermore, the global spread of resistant bacterial strains through international travel and trade underscores the need for a coordinated and multifaceted approach to combatting azithromycin resistance. Addressing these factors requires a comprehensive strategy that encompasses improved surveillance, antibiotic stewardship programs, public education campaigns, and regulatory measures to ensure the prudent use of azithromycin and other antibiotics. By understanding and mitigating the various drivers of resistance, we can work towards preserving the effectiveness of azithromycin and safeguarding public health.
Implications of Azithromycin Resistance on Public Health
Azithromycin resistance poses a significant threat to public health, leading to challenges in treating bacterial infections effectively. Without proper intervention, the spread of azithromycin-resistant bacteria can result in more severe illnesses, prolonged treatment durations, higher healthcare costs, and increased mortality rates. The overuse and misuse of azithromycin contribute to the development of resistance, emphasizing the need for strategic actions to preserve the efficacy of this vital antibiotic and safeguard public health. Implementation of robust surveillance measures, antimicrobial stewardship programs, and education initiatives are crucial in mitigating the impact of azithromycin resistance and maintaining effective treatment options for bacterial infections.
Strategies for Combating Azithromycin Resistance

Strategies for combating Azithromycin resistance involve a multi-faceted approach that addresses both the overuse and misuse of this antibiotic. Implementing antibiotic stewardship programs is crucial in promoting appropriate Azithromycin use and reducing the development of resistance. Additionally, raising awareness among healthcare providers and the general public about the importance of proper antibiotic usage can contribute significantly to combating resistance. Encouraging the use of alternative treatment options when appropriate, along with rigorous surveillance of antibiotic resistance patterns, can also play a pivotal role in managing Azithromycin resistance effectively. Emphasizing the need for collaboration between healthcare professionals, researchers, policymakers, and the pharmaceutical industry is vital in developing comprehensive strategies to combat Azithromycin resistance.
Role of Antibiotic Stewardship Programs in Prevention
Antibiotic stewardship programs play a crucial role in combating azithromycin resistance by promoting responsible use of antibiotics. These programs involve multidisciplinary teams working together to optimize antibiotic prescribing, ensuring that patients receive the right antibiotics at the right dose and duration. Through education, guidelines, and monitoring, stewardship programs help healthcare providers make informed decisions, reducing unnecessary antibiotic use and minimizing the development of resistance. By integrating stewardship principles into clinical practice, healthcare facilities can enhance patient outcomes and contribute to the global effort to preserve the effectiveness of azithromycin and other vital antibiotics.
| Antibiotic Stewardship Programs | Key Components |
|---|---|
| Educational Initiatives | Training healthcare providers on proper antibiotic use |
| Guidelines Development | Establishing protocols for antibiotic prescribing |
| Monitoring and Feedback | Regularly assessing and optimizing antibiotic practices |
Future Directions in Addressing Azithromycin Resistance
In looking ahead to addressing Azithromycin resistance, the field of antibiotic research is poised for groundbreaking developments. Collaborative efforts among scientists, healthcare providers, and policymakers will be crucial in formulating innovative solutions. By leveraging cutting-edge technologies, such as precision medicine and genomic analysis, researchers can tailor treatments to combat resistant strains effectively. Moreover, enhancing global surveillance systems and promoting antimicrobial stewardship programs will be pivotal in preserving the efficacy of Azithromycin and other crucial antibiotics. Embracing a proactive approach that anticipates future challenges and adapts swiftly will be paramount in staying ahead of emerging resistance patterns. Through a unified and forward-thinking strategy, the medical community can pave the way for a sustainable future in combating Azithromycin resistance.
California law requires employers to pay for all appropriate medical treatment for on-the-job injuries.
To report provider listing inaccuracies, contact the MPN contact at 1-877-775-7772 or mpnhelp@medexhco.com
To contact the MPN contact, call 1-877-775-7772 or mpnhelp@medexhco.com
To contact the Medical Access Assistant, call 1-888-509-1474 or MAA@medexhco.com
To obtain a copy of any notification regarding the MPN, including the Complete Employee Notification, please contact the claims administrator for your claim. If you need assistance identifying or contacting the claims administrator on your claim, please contact the Medical Access Assistant at 1-888-509-1474 or MAA@medexhco.com. We may be able to help you connect to the appropriate party.
© 2024 MEDEX · MEDEX The Total Solution to Rising Workers' Compensation Costs
Conditions of Use • Privacy Policy

